Evaluation of the Spectrum Of Co-Existing Injuries In Patients With Maxillofacial Trauma: A Retrospective Study
Dr. Rajesh. P1, Dr. Vaishali. V2*
1 Professor and Head, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai, India.
2 Post Graduate, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai, India.
*Corresponding Author
Dr. Vaishali. V, BDS,
Department of Oral and Maxillofacial surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai- 603103, India.
Tel: 8056379290, 8838017051
Email: vaish712.venkat@gmail.com
Received: December 19, 2021; Accepted: January 24, 2022; Published: January 25, 2022
Citation: Dr. Rajesh. P, Dr. Vaishali. V. Evaluation of the Spectrum Of Co-Existing Injuries In Patients With Maxillofacial Trauma: A Retrospective Study. Int J Surg Res. 2022;8(1):152-155. doi: dx.doi.org/10.19070/2379-156X-2200033
Copyright: Dr. Vaishali. V© 2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To evaluate the types and frequency of co-existing injuries in patients sustaining maxillofacial trauma in a tertiary care centre of Tamil Nadu.
Settings: Trauma, being referred as silent epidemic of the era, potentially results in millions of death every year worldwide.
The maxillofacial surgeon, being a part of the trauma team, gets to examine the patient first hand and thus has a shared responsibility
to thoroughly assess the injuries incurred by other systems in addition to the survey of maxillofacial injuries. This study
intends to highlight the need for an interdisciplinary management model in approaching facial trauma.
Methods: A retrospective analysis of 888 maxillofacial trauma cases reported to the emergency department during the last
five years was done. Detailed review of primary and secondary survey was done. Age, gender, mechanism of injury, type and
frequency of fracture, type and frequency of concomitant injury were recorded and subjected to statistical analysis.
Result: Associated injuries were sustained by 329 patients. Majority sustaining injuries were 20- 39 years and predominantly
males. Soft tissue injury was frequently observed. Mandibular fractures were the most common among the hard tissue injury.
Concomitant injuries observed in descending order was Neurologic, Orthopaedic, Ophthalmologic, Chest and finally abdominal.
Conclusion: Sound knowledge on the type and severity of associated injuries of other systems is mandatory for every surgeon
to keep any latent life threatening conditions at the surgeons catch.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Maxillofacial; Trauma; Concomitant Injuries; Traumatic Brain Injury; Oral Surgery.
Introduction
Patients with maxillofacial injuries are mostly seen to have co-existing
injuries resulting from the trauma. The extent and degree of
these injuries depend on the mechanism and impact of the trauma.
The proficiency, with which a definite assessment is made, is a
major factor in the prognosis of the patient [3]. Treatment of the
maxillofacial injuries would be complex without a comprehensive
perception of the damage incurred by other systems in the body
of the victim [1]. There is increasing recognition that patients,
who have sustained multiple injuries, benefit from early multidisciplinary
management by a specialized unit, or trauma centre [2].
It is required of the maxillofacial surgeon attending such cases in
the emergency department to promptly identify these concomitant
injuries during the primary and secondary survey to avoid
grave situations. This study intends to identify commonly occurring
collateral injuries with maxillofacial trauma to render a directed
patient care.
Materials and Methods
A retrospective analysis of a total of 6350 trauma patients, reported
to the emergency department of our institution during
the five year period, of March 2015 - March 2020, was carried
out. Of these, a detailed review of 888 patients with maxillofacial
trauma was done and data regarding age, gender, type of injury
and its frequency, mechanism of injury, concomitant injuries of
other organ systems and their frequencies was recorded. Patients
with complete medical records along with radiologic records were
included in the study. Maxillofacial injuries were recorded as soft tissue injuries, fractures of the mandible, maxilla, zygomaticomaxillary
complex, combined mandibular and middle third region
and pan facial based on the clinical and radiological medical
records. Concomitant injuries included are the neurological
including traumatic brain injury, cervical spine injury, Orthopaedic,
Ophthalmologic, Chest or pulmonologic, abdominal injuries.
Records pertaining to the concomitant injuries were either taken
from their emergency survey, or opinion obtained prior to the
treatment for maxillofacial injury or treatment record attributing
to the management of those specific system injuries. Cases with
missing or incomplete medical records were excluded from the
study. The data was tabulated and subjected to statistical analysis.
Statistical Analysis
SPSS software version 21 was used. Chi square test was applied
and to assess the relationship between the variables Pearson’s
Correlation was used. In all the above probability value .05 is considered
as significant level.
Results
A total of 888 maxillofacial trauma patients were identified for
the study. 529(59.6 %) of them belonged to 20-39 years of age,
the maximum number to experience maxillofacial trauma followed
by 40- 60 years with a total number of 194 (21.6%), with
134 (15.1%) less than 18 years and finally above 60 years with
31(3.5%) numbers. 673 (75.8%) were males and 215 (24%) females.
There were a total of 343 hard tissue and 545 soft tissue
maxillofacial injuries present. Mandibular fractures (148) were the
most frequent, followed by zygomatico maxillary complex (77),
combined mandibular-middle third (67), isolated maxillary (37)
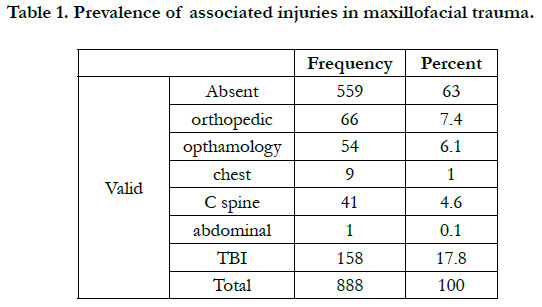
and pan facial fractures (17). Out of the 888 maxillofacial trauma
patients, 329 (37%) of them sustained associated injuries of other
systems along with maxillofacial injuries. About 17.8% of them
had traumatic brain injuries, 4.6% had cervical spine injuries, 7.4
% had orthopaedic injuries, 6.1% had ophthalmologic injuries,
1% had chest injuries and 0.1% had abdominal injuries (Table
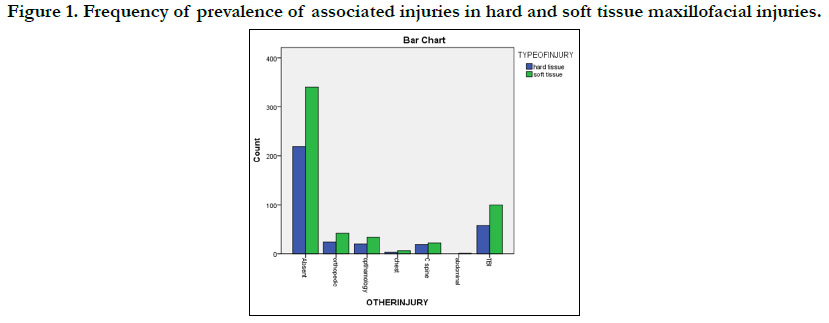
1). Prevalence of different injuries with respect to hard and soft
tissue maxillofacial injuries has been depicted in Figure 1. No statistical
significance between the type of maxillofacial injury and
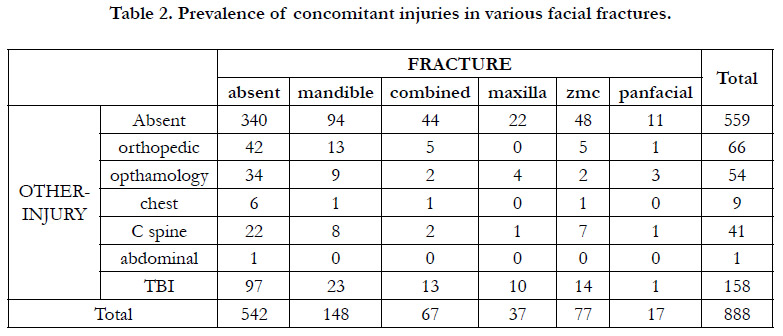
prevalence of associated injuries was found. Frequency of occurrence
of the concomitant injuries in different types of facial
fractures was analysed and depicted in Table 2. Highest number
of traumatic brain injuries were found with middle third fractures
when compared to mandibular fractures, cervical spine injuries
was highest in mandibular fractures, orthopaedic injuries in mandibular
fractures and ophthalmologic injuries in middle third fractures.
Figure 1. Frequency of prevalence of associated injuries in hard and soft tissue maxillofacial injuries.
Discussion
Nowadays, facial injuries have become a quotidian situation in the
emergency rooms as face is highly vulnerable to trauma due to
the fact that it is the most exposed region of our body [3]. It
has been reported that about 50% of head and neck collateral
injuries were observed in all trauma deaths [1]. This study aimed
at illustrating the multisystem nature of the traumatic injuries associated
with the fractures of facial skeleton. It is expected of the
high energy forces causing facial fractures to have caused injuries
to the other organ systems also. The extent and type of these
injuries however depends on the mechanism of injury, force and
its impact, patient factors like age, gender, co-existing morbidities
etc. The diagnosis of such injuries has to be done on time and a
coordinated interdisciplinary management protocol will have to
be formulated in treating a poly trauma patient. While enormous literature is available in assessing the existence of maxillofacial
fracture in poly-trauma, scarce is the information validating the
converse hypothesis. This study is designed with the aim of correlating
the other injuries existing in maxillofacial trauma since
maxillofacial surgeons form a part of the integrated trauma team
that encounters the patient first hand after the injury. Thus it is
imperative for every maxillofacial surgeon to be aware of the expected
accessory injuries that has to be addressed during the primary
and secondary survey.
In our study, the mean age group 31.40 of which 673 were males
and 215 were females. No significant statistical correlation was
found between the prevalence of concomitant injuries and, age
and gender of the study population. Road traffic accident was
the commonest cause followed by interpersonal violence and the
others. This was in accordance with the study by Deliverska et al,
Follmar et al [5], where they discussed possible random pattern
of mechanical trauma, with forces distributed to the entire body
that is conducive to injury to multiple parts of the body. With this
opinion, on correlating the existence of associated injuries to the
mechanism of trauma, Road traffic accident proves to cause poly
trauma than the assault since the latter is directed to a particular
portion of the body. . In our study most common fracture was
mandibular (16%), followed by ZMC (8.6%), combined mandibular
and middle third (7.5%), isolated maxillary (4.16%), pan facial
(1.9%), soft tissue injury (61%). Among the associated injuries,
in the descending order is the neurological including Traumatic
Head Injury and Cervical spine injury, followed by Orthopaedic,
ophthalmologic, pulmonologic and abdominal injuries.
Frequently occurring concomitant injury in our study was Traumatic
Head Injury (17.8%) which varied between mild, moderate
and severe injuries. Maxillofacial injuries comprising hard tissue as
well as soft tissue injuries can be associated with traumatic brain
injuries due to the impact of forces transmitted through the head
and neck [8]. Davidoff et al found a strong association of traumatic
head injuries with facial fractures while Haug et al reported
76% incidence of traumatic brain injuries with maxillofacial fractures.
In our study 46.7% of 124 cases of facial fractures presented
with traumatic brain injuries. Higher prevalence rate could
be related with middle face injuries owing to the complexity of
anatomy with lesser density of the bones and its proximity to the
skull. 4.6 % of the sample sustained cervical spine injuries along
with maxillofacial fractures. Hackl et al reported a rate of 19.2%
of prevalence of cervical spine injuries in their study while several
authors have reported a prevalence rate ranging between 0 to
4.3% [4]. Generally a maxillofacial trauma patient is assumed to
have sustained cervical spine injuries unless proven otherwise. If
the neurologic status of the patient with respect to injury of brain
and cervical spine could not be discretely ruled out, it is mandatory
to go for radiologic imaging prior to maxillofacial management
protocol. All the procedures should be deferred until the
patient is found neurologically stable. The pattern and severity
of these injuries highly influences the management protocol and
hence should be ruled out with utmost importance.
Neurologic injuries are succeeded by orthopaedic injuries with
7.4% of total coexisting injuries. Deliverske et al reported 22% of
orthopeadic injuries in patients with maxillofacial fractures which
supports the results of our study that had 29.7% of the total facial
fractures. This could be attributed again to multisystem involvement
of a serious trauma and its impact. Often these injuries do
not contra indicate timely management of maxillofacial injuries
and if needed, interdisciplinary simultaneous surgical management
has also been opted by the surgeons. But such decisions
purely depends on the type of procedures, duration of surgery,
general status of the patients, anticipated complications like intraoperative
blood loss or hypothermia and fitness of the patient
for anaesthetic procedures.
Ophthalmologic injuries form a significant proportion of this lot
(6.1%). These occur often as a complication of upper and middle
third fractures especially orbito- zygomatico- maxillary complex
fractures. Precise evaluation of changes in ocular structure and
function is of prime importance to alleviate the risk of morbidity
in the future. Pulmonologic injuries form of the total injuries.
Though relatively lower in number than the others stated, missed
diagnosis of the chest injuries often puts the patient’s life at risk.
Pulmonologic injuries can vary from fracture of the sternum or
rib to injury to the tissues of the lungs. Chest x-ray plays an inevitable
role in the preliminary assessment of a poly trauma patient
and if required higher imaging modality like CT or MRI can be
preferred. Often these injuries are associated with severely injured
trauma patients. Abdominal injuries are insignificant in values but
do occur in rare cases. But one should be cautious and be aware
of such occurrences so as to combat such unforeseen emergencies
if occurs.
Except for the neurological status, other injuries don’t cause significant
delay in the fractures of the facial skeleton. The results
of the study highlights the relatively high prevalence of collateral
injuries proves to be a reminder of acuity of these patients and need for a multidisciplinary approach to the trauma for rendering
directed comprehensive care in whole, volume after initial stabilization
of the patient. Precautious examination and identification
is expected of the surgeon. Most importantly, fractures from
road traffic accident should never be imagined as an isolated injury
but a part of spectrum of significant critical injury requiring
system by system assessment. Based on the results of the present
study, coexisting injuries in areas other than the face in poly
trauma patients should be expected first and foremost as trauma
that involves sufficient energy to fracture the bones of the facial
skeleton is also likely to distribute a substantial amount of force
to other parts of the body, and thus cause injury.
Conclusion
Knowledge of the frequency of concomitant injuries existing
with the maxillofacial injuries post trauma serves as guidance to
prompt identification and comprehensive management of the patient.
Also it emphasises not to narrow down the focus on maxillofacial
region but to widen the thoroughness of the assessment
to the other systems that could potentially lead to catastrophic
consequences if neglected.
References
- Scherbaum Eidt JM, De Conto F, De Bortoli MM, Engelmann JL, Rocha FD. Associated injuries in patients with maxillofacial trauma at the hospital são vicente de paulo, passo fundo, Brazil. J Oral Maxillofac Res. 2013 Oct 1;4(3):e1.Pubmed PMID: 24422034.
- Down KE, Boot DA, Gorman DF. Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg. 1995 Dec;24(6):409-12.Pubmed PMID: 8636636.
- Patil SG, Munnangi A, Joshi U, Thakur N, Allurkar S, Patil BS. Associated Injuries in Maxillofacial Trauma: A Study in a Tertiary Hospital in South India. J Maxillofac Oral Surg. 2018 Dec;17(4):410-416.Pubmed PMID: 30344378.
- Roccia F, Cassarino E, Boccaletti R, Stura G. Cervical spine fractures associated with maxillofacial trauma: an 11-year review. J Craniofac Surg . 2007 Nov 1;18(6):1259-63.
- Follmar KE, DeBruijn M, Baccarani A, Bruno AD, Mukundan S, Erdmann D, et al. Concomitant injuries in patients with panfacial fractures. J Trauma Acute Care Surg. 2007 Oct 1;63(4):831-5.
- Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003 Jan;113(1):102-6.
- Carlin CB, Ruff G, Mansfeld CP, Clinton MS. Facial fractures and related injuries: a ten-year retrospective analysis. J Craniomaxillofac Trauma. 1998 Summer;4(2):44-8.Pubmed PMID: 11951431.
- Rajandram RK, Syed Omar SN, Rashdi MF, Abdul Jabar MN. Maxillofacial injuries and traumatic brain injury--a pilot study. Dent Traumatol. 2014 Apr;30(2):128-32.Pubmed PMID: 23782407.
- Davidoff G, Jakubowski M, Thomas D, Alpert M. The spectrum of closedhead injuries in facial trauma victims: incidence and impact. Ann Emerg Med. 1988 Jan;17(1):6-9.Pubmed PMID: 3337417.
- Ajike SO, Adebayo ET, Amanyiewe EU, Ononiwu CN. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. Niger J Surg Res. 2005;7(3):251-5.
- Obuekwe ON, Etetafia M. Associated injuries in patients with maxillofacial trauma. Analysis of 312 consecutive cases due to road traffic accidents. J Med Biomed Res. 2004 Jun;3(1):30-6.
- McGoldrick DM, Fragoso-Iñiguez M, Lawrence T, McMillan K. Maxillofacial injuries in patients with major trauma. Br J Oral Maxillofac Surg. 2018 Jul 1;56(6):496-500.
- Singaram M, G SV, Udhayakumar RK. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. J Korean Assoc Oral Maxillofac Surg. 2016 Aug;42(4):174-81. Pubmed PMID: 27595083.
- Fama F, Cicciu M, Sindoni A, Nastro-Siniscalchi E, Falzea R, Cervino G, et al. Maxillofacial and concomitant serious injuries: An eight-year single center experience. Chin J Traumatol. 2017 Feb;20(1):4-8.Pubmed PMID: 28209449.
- Pungrasmi P, Haetanurak S. Incidence and etiology of maxillofacial trauma: a retrospective analysis of King Chulalongkorn Memorial Hospital in the past decade. Asian Biomed. 2017 Aug 1;11(4):353-8.
- Reich W, Surov A, Eckert AW. Maxillofacial trauma - Underestimation of cervical spine injury. J Craniomaxillofac Surg. 2016 Sep;44(9):1469-78. Pubmed PMID: 27527678.
- Choonthar MM, Raghothaman A, Prasad R, Pradeep S, Pandya K. Head injury-a maxillofacial surgeon’s perspective. J Clin Diagn Res. 2016 Jan;10(1):ZE01.