A Case Series Of Gingival Hyperpigmentation Treatment Using Laser And Scalpel Techniques
Bhargavi Sheth1, Poonam Rai1*, Devanand Shetty2, Kushal Shah1
1 Post Graduate Student, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
1 Professor, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
2 Professor & Head of Department, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
*Corresponding Author
Dr. Poonam Rai,
Professor, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
Tel: +91 98920 19346
E-mail: drpoonamm.singh@gmail.com
Received: December 13, 2021; Accepted: February 12, 2022; Published: February 18, 2022
Citation: Bhargavi Sheth, Poonam Rai, Devanand Shetty, Kushal Shah. A Case Series Of Gingival Hyperpigmentation Treatment Using Laser And Scalpel Techniques. Int J Dentistry Oral Sci. 2022;9(2):5242-5245. doi: dx.doi.org/10.19070/2377-8075-220001051
Copyright: Poonam Rai©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The hyper-pigmentation in the gingiva is usually seen because of the excessive and unusual collection of melanin in the gingiva and presents as a darkened appearance of the gingival tissue. This abnormal gingival pigmentation usually jeopardizes smile and facial aesthetics and can be seen because of various physiological disarray. Various modalities to treat this condition are available. In this case series, effort has been made to assess the techniques of melanin depigmentation using conventional scalpel and laser method.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Melanin Hyperpigmentation; Aesthetics; Laser; Scalpel; Dark Gums.
Introduction
In dentistry, aesthetics plays an important role. The health of the
gingiva and it’s appearance are essential components of aesthetics.
1 Gingiva being the most common intraoral tissue affected by
excessive melanin pigmentation, results in an unpleasant look.
Melanin hyperpigmentation is frequently seen in the gingival tissue
due to unusual deposits of melanin and even though it is not
a medical issue to worry about, practitioners frequently face challenges
of successfully bringing about aesthetics of the gingiva.
Melanin, a brownish pigment, is the most common cause of endogenic
pigmentation of the gingiva and is the chief pigment of
the mucosa. In the gingiva, it is seen in all ethnicities. This brownish
or dark-black pigmentation and discolouration of the gingiva
can be brought about by a variety of local and systemic factors.2
Long term usage of certain medicines, genetic component, systemic
conditions such as, Albright’s syndrome; endocrine disturbances,
chronic pulmonary disease, hemochromatosis and racial
pigmentation are known causes of oral melanin pigmentation.
Tobacco use is a common cause3,4among local factors.
Today's evolving aesthetic worries amongst the patients call for
the removal of unpleasant hyper pigmented gingiva in order to
create an aesthetically pleasing smile.
Case Series
Following cases were taken from the outpatient periodontics department.
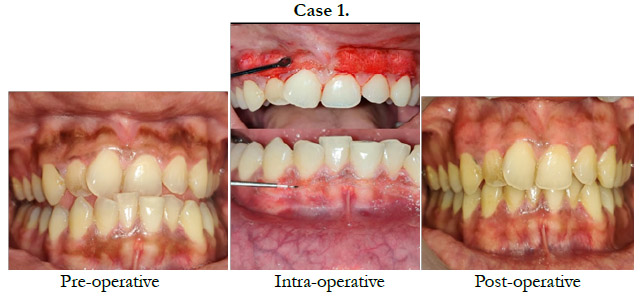
Case 1
A 22 year old female patient complained of brownish gums. She
asked for surgical management through which her smile and aesthetics
could be enhanced. Patient was fit medically and upon oral
examination, scattered melanin hyperpigmentation in the attached
gingiva both in the maxillary and mandibular arch was seen.
Keeping in mind the concern expressed by the patient about her
unesthetic looks it was decided to perform gingival depigmentation
procedure using scalpel technique in the maxilla and laser
technique in the mandible.
Case 2
A 18 year old female patient visited with a primary complaint of
blackish gums. On examining, it was seen that she had diffuse
melanin hyperpigmentation in the attached gingiva both in the
maxillary and mandibular arch.
The patient was worried about the condition and asked for aesthetic
treatment.
Keeping in mind the worries shown by the patient about her unpleasant
smile it was decided to perform a depigmentation procedure
of the gingival tissues using scalpel technique in the maxilla
and laser technique in the mandible.
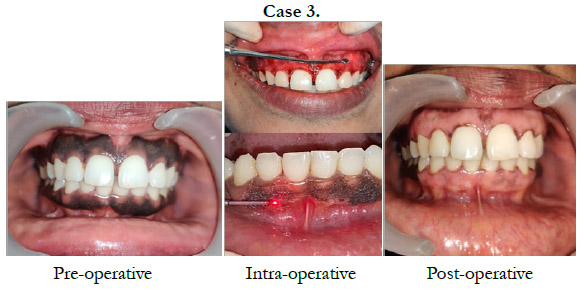
Case 3
A 46 year old patient visited with the primary complaint of dark
gums. Oral examination showed heavily pigmented attached gingiva
in both the maxilla and the mandible.
The patient requested for aesthetically better gums.
Keeping the concern of the patient In mind regarding her unpleasant
appearance it was decided to carry out gingival depigmentation
using scalpel technique in the maxilla and laser technique
in the mandible.
Surgical Technique
In all three cases, before the start of the surgery, a detailed medical
history and haematological investigation was done to rule out
any contraindication for the surgery. Gingival depigmentation was
planned based on the patient’s concern. The entire procedure was
explained to each of the patient and written consents were taken.
Oral prophylaxis was carried out on all the three patients and oral
hygiene instructions were given.
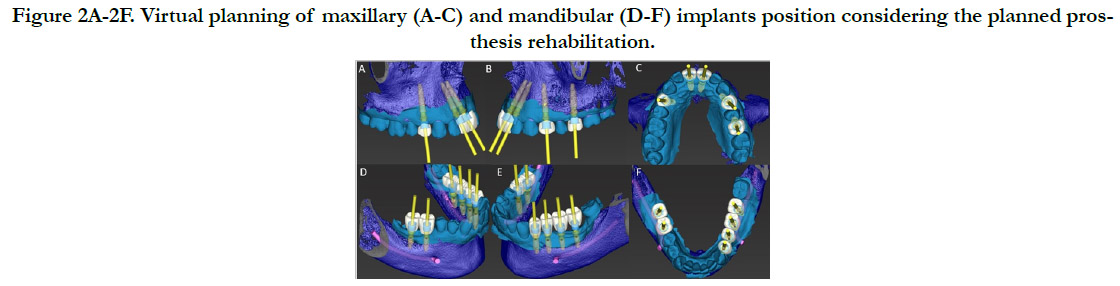
In The Maxilla
From the distal region of the right canine (13) to distal region of
the left canine (23) in the anterior maxilla, regional anaesthesia
was administered. A bard parker handle with a no. 15 blade was used to remove the pigmented layer. After removing the visible
pigmented epithelium along with a thin layer of connective tissue
with the scalpel, the exposed surface was irrigated with saline.
Coe-pack was placed at the operated site for 1 week.
In The Mandible
From the distal region of the right canine (43) to distal region of
the left canine (33) in the anterior mandible, regional anaesthesia
was administered.
A diode surgical laser Biolase Soft Tissue Diode Laser – EPIC X
with a 400 micron tip and 1 W power was initiated and laser ablation
was done from the mucogingival junction towards the free
gingival margin including the papillae in a pulsed mode. Ablation
was performed in light brushing stokes and remnants of ablated
tissue was removed using sterile gauze dampened with saline solution.
Protective eyeglasses were worn by the patient and the staff
to fulfil the Food and Drug Administration laser safety rules.
The depigmentation procedure was carried out till no pigments
were visible. Coe-pack was placed at the surgical area for 1 week.
Medication
In all three cases, the patients were prescribed analgesics Upto 5
days post-operatively.
Results
Patients were reviewed at the end of 24 hours followed by one
week, one month and three months. At every visit, the operated
area was irrigated with 1% povidone iodine4 after which the pain
scores using the Present Pain Intensity Scale5 and the soft tissue
healing using the Wound Healing Index6 were recorded.
After 24 hours, the patients experienced a pain score of 1(mild
pain) following the scalpel technique in the maxillary arch and
a pain score of 0(no pain) following the laser technique in the
mandibular arch.
According to the WHI, at the end of 24 hours, the patients
showed a score of 2(slight gingival oedema, erythema, and discomfort)
following the scalpel technique in the maxillary arch and
a score of 1(absence of gingival oedema, erythema, suppuration
and discomfort) following the laser technique in the mandibular
arch.
Following this, the patients experienced a pain score of 0 with
both the scalpel technique and laser technique in the maxillary
and mandibular arch respectively at the end of one week, one
month and three months.While recording the soft tissue healing,
a score of 1 was given following both the scalpel technique and
laser technique in the maxillary and mandibular arch respectively
at the end of one week, one month and three months.
To summarize, uneventful healing took place and no complications
were seen post-operatively. All the patients experienced mild
pain on the first day following conventional scalpel technique in
the maxilla and no pain following the laser technique in the mandible.
At the end of one week the gingiva was re-examined. It was
healthy, firm and resilient. At the end of one month, complete reepithelisation
had taken place and the cases were evaluated again
at the end of three months. The patients were satisfied over the
improved colour of the gingiva.
Discussion
Components of an attractive smile largely depend on the health
and appearance of the gingiva. The gingival colour has a tremendous
effect on not only the smile but also facial aesthetics1.As
seen, it differs from individual to individual depending on its location
in the oral cavity and seems to be correlated with the colour
of the skin1.
The present study showed that both laser and scalpel technique
showed favourable results in terms of bleeding, healing, discomfort,
pain and re-pigmentation and is consistent with an article
given by Harpreet S. while assessing the pain score following gingival
depigmentation using laser and scalpel technique where no
statistical significance was found between the two groups10.
However studies by Khalilian F7 and Girish S9. Comparing the
efficacy of laser to conventional scalpel technique in gingival depigmentation
showed reduced pain experienced by the patient
and better operator comfort in the laser group compared to the
scalpel group.
Depigmentation of the gingiva is a periodontal cosmetic surgical
procedure wherein the abnormal and excessive pigmentation
in the gingiva is removed or reduced by different techniques like
conventional scalpel technique, Abrasion technique, Electro surgery,
Cryosurgery, Laser, Radiosurgery, chemicals such as phenols
and citric acid, Acellular dermal matrix autograft8.
The limitation of the study is that a larger sample has to be selected
in order to determine the effectiveness of each technique in
terms of bleeding, healing, discomfort, pain and re-pigmentation.
Conclusion
This study brings us to the conclusion that both conventional
scalpel technique and laser technique gave results which are aesthetically
acceptable with least discomfort to the patients. Epithelialization
was complete and uneventful healing took place. There
was no reappearance of pigments in both scalpel and laser technique
at the end of third month.
References
-
[1]. Doshi Y, Khandge N, Byakod G, Patil P. Management of gingival pigmentation
with diode laser: is it a predictive tool. Int J Laser Dent. 2012
Jan;2(1):29-32.
[2]. Malhotra S, Sharma N, Basavaraj P. Gingival esthetics by depigmentation. J Periodontal Med Clin Pract. 2014;1(1):79-84.
[3]. Porter SR, Flint SR, Scully C. Oral Diseases. Martin Dunitz, second edition, London.1996,1-371.
[4]. Domingo MA, Farrales MS, Loya RM, Pura MA, Uy H. The effect of 1% povidone iodine as a pre-procedural mouthrinse in 20 patients with varying degrees of oral hygiene. J Philipp Dent Assoc. 1996 Sep-Nov;48(2):31-8. Pubmed PMID: 9462082.
[5]. Sirintawat N, Sawang K, Chaiyasamut T, Wongsirichat N. Pain measurement in oral and maxillofacial surgery. J Dent Anesth Pain Med. 2017 Dec;17(4):253-263.Pubmed PMID: 29349347.
[6]. Marini L, Rojas MA, Sahrmann P, Aghazada R, Pilloni A. Early Wound Healing Score: a system to evaluate the early healing of periodontal soft tissue wounds. J Periodontal Implant Sci. 2018 Oct 24;48(5):274-283.Pubmed PMID: 30405935.
[7]. Khalilian F, Nateghi Z, Janbakhsh N. Gingival Depigmentation Using Lasers: A Literature Review. Br J Med Med Res. 2016;12:1-7.
[8]. Murthy MB, Kaur J, Das R. Treatment of gingival hyperpigmentation with rotary abrasive, scalpel, and laser techniques: A case series. J Indian Soc Periodontol. 2012 Oct;16(4):614-9.Pubmed PMID: 23493062.
[9]. Suragimath G, Lohana MH, Varma S. A Split Mouth Randomized Clinical Comparative Study to Evaluate the Efficacy of Gingival Depigmentation Procedure Using Conventional Scalpel Technique or Diode Laser. J Lasers Med Sci. 2016 Fall;7(4):227-232.Pubmed PMID: 28491257.
[10]. Grover HS, Dadlani H, Bhardwaj A, Yadav A, Lal S. Evaluation of patient response and recurrence of pigmentation following gingival depigmentation using laser and scalpel technique: A clinical study. J Indian Soc Periodontol. 2014 Sep;18(5):586-92.Pubmed PMID: 25425820.