Elimination Of Post-Extraction Atrophy And Deformation Of The Alveolar Part Of The Jaw By Injecting Osteoplastic Materials
Bezrukov S.G1, Shepelev A.A2, Bezrukov G.S3, Odilbekov U.A4, Yelcheva L.A5*
1 Head of the Department of Surgical Dentistry and Maxillofacial Surgery, Professor, Faculty of Dentistry of the Medical Academy named after S. I.
Georgievsky of Vernadsky CFU, Simferopol, 95000, Russian Federation.
2 Surgeon Dentist-Implantologist, Dental Clinic "Apex-Plus", Sevastopol, 99000, Russian Federation.
3 Docent of the Department of Pediatric Dentistry, Faculty of Dentistry of the Medical Academy named after S. I. Georgievsky of Vernadsky CFU.
Simferopol, 95000, Russian Federation.
4 Resident Faculty of Dentistry of the Medical Academy named after S. I. Georgievsky of Vernadsky CFU, Simferopol, 95000, Russian Federation.
5 Senior Teacher of the Department of Surgical Dentistry and Maxillofacial Surgery, Faculty of Dentistry of the Medical Academy named after S. I.
Georgievsky of Vernadsky CFU, 95000, Russian Federation.
*Corresponding Author
Yelcheva L.A,
Senior Teacher of the Department of Surgical Dentistry and Maxillofacial Surgery, Faculty of Dentistry of the Medical Academy named after S. I. Georgievsky of Vernadsky CFU,
95000, Russian Federation.
Tel: +79787253877
E-mail: lidayelcheva@gmail.com
Received: September 18, 2021; Accepted: November 13, 2021; Published: November 23, 2021
Citation: Bezrukov S.G, Shepelev A.A, Bezrukov G.S, Odilbekov U.A, Yelcheva L.A. Elimination Of Post-Extraction Atrophy And Deformation Of The Alveolar Part Of The Jaw By Injecting Osteoplastic Materials. Int J Dentistry Oral Sci. 2021;8(11):5101-5103. doi: dx.doi.org/10.19070/2377-8075-210001026
Copyright: Yelcheva L.A©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Post-extraction atrophy and deformation of the alveolar ridge of the jaws continues to be a serious problem in dentistry. Surgical treatment of these conditions is associated with the need to use autoplastic material, which causes certain difficulties. The injectable route of administration of osteoplasts seems to be less traumatic. However, to date, it has not found its wide application. The aim of the study was to evaluate the effectiveness of the method of eliminating post-extraction atrophy and deformation of the alveolar process by injecting osteoplastic materials on the example of platelet-rich autoplasma (PRP) and a suspension of a synthetic osteoplastic drug (Collapan). 68 patients with a limited postextraction defect or atrophy of the alveolar part of the jaw were treated and examined. Osteoplastic materials (PRP and Collapan) were injected into the bone defect area under the periosteum. In the conditions of the clinic, the effectiveness of the proposed injection method of combined administration of osteoplastic materials was established, which is expressed in the activation of bone regeneration processes with partial restoration of the lost volumes of the alveolar ridge, which is achieved due to the increased concentration in PRP of a complex of growth factors that ensure the implementation of the osteoinductive functions of the used graft, as well as the osteoconductive effect of a synthetic bioresorbable bone drug (Collapan).
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Postextraction Atrophy And Deformation Of The Alveolar Ridge; Treatment; Osteoplastic Materials; Injection
Route Of Administration.
Introduction
One of the main tasks of modern dentistry is to restore the integrity
of the dentition and the function of chewing. Prosthetic
dentistry, having reached a high level in the use of modern technologies
in the manufacture of permanent structures and removable
dentures, is not always able to effectively solve the tasks, due
to the fact that this is prevented by post-extraction atrophy and
deformation of the alveolar ridge of the jaw. It is known that
within the first year after tooth extraction, the alveolar process
loses up to 70% of the bone tissue volume, which leads to a decrease
in the aesthetics of permanent structures and the fixation
of removable ones, and also often are a contraindication to the
use of dental implantation. Surgical removal of postextraction atrophy
and deformation of the alveolar part of the jaw is widely
used for pre-prosthetic and pre-implantation preparation of a
dental patient with both generalized and local (in the projection
of 1-3 teeth) pronounced bone tissue deficiency [7]. However,
this method has significant limitations due to the need for the
preparation and use of autografts [1, 2, 8]. The injectable route
of administration of osteoplasts seems to be less traumatic. At
the same time, to date, it has not found its wide application. The optimal dosage and depth of the location of osteoplastic materials
have not been clarified. In addition, the effectiveness of both
monotherapy and combined use of bone regenerants during their
injection has not been studied [3].
The purpose of the study. Evaluation of the effectiveness of the
method for eliminating post-extraction atrophy and deformation
of the alveolar ridge of the jaw by subperiosteal injection of osteoplastic
materials on the example of platelet-rich autoplasma
(PRP) and a suspension of a synthetic osteoplastic drug (Collapan).
Materials And Methods
68 patients with a limited postextraction defect or atrophy of the
alveolar part of the jaw were treated and examined. In the control
group (n=30), correction of the shape of the alveolar process was
performed using subperiosteal injections of platelet-rich plasma.
Depending on the prevalence of the sections of local bone atrophy,
from 2 to 4 ml of PRP was administered simultaneously. In
the main group (n=38), local injectable augmenting therapy was
carried out by combined subperiosteal administration of PRP and
a suspension of a synthetic osteoplastic drug (Collapan). At the
same time, osteoplasts were used separately in equal doses. Primarily,
plasma enriched with platelets (1-2 ml) was injected and
then (after 1-2 minutes) a suspension of fine powder Collapan
was placed under the periosteum in an isotonic sodium chloride
solution (in a ratio of 1:2) with a volume of 1-2 ml. All manipulations
were performed under infiltration local anesthesia with 0.5
% lidocaine solution (2-3 ml). To achieve the planned therapeutic
osteoplastic result, the patients underwent additional injection
procedures (but no more than three), with a break of 2 weeks.
Platelet-rich plasma was obtained from the patient's blood, which
was taken from the ulnar vein with a disposable needle - catheter
into 2-4 sterile vacuum tubes (9 ml each). Such a volume of
blood loss (only from 18 to 36 ml) is considered insignificant, it
is mild by the patient, does not require the appointment of additional
therapy. To inhibit hemocoagulation, 0.05 ED of heparin
was previously injected into each tube. Hermetically sealed containers
were placed in a centrifuge (Hettich Eva-20, Germany).
The blood was centrifuged in two stages: 10 minutes at 2000 rpm
(plasma with a low platelet content was obtained in the upper layer
and taken with a syringe), then another 15 minutes at 4000 rpm
(plasma enriched with platelets was collected in the upper layer, it
was also collected in a syringe). 1-1.3 ml of PRP was taken from
each tube. The resulting material was injected subperiosteally using
an insulin syringe (1 ml volume) with a non-removable needle.
Patients in the main group, the PRP was prepared by the above
procedure, but was introduced into the subperiosteal space at half
the dose (in comparison with the control group), followed by a
second syringe through a needle with a wide diameter (0.5 mm) in
the same plot were injected the same amount of a suspension of
fine osteoplastic powder (Collapan) in isotonic sodium chloride
solution (ratio 1:2).
The basis of the methods of treatment used in our work, lay
down recommendations for the use of PRP present in the available
literature and instructions for use of the drug Collapan [3-6,
9].
Stomatological examination of patients included examination of
the face and dentition. During the treatment, attention was paid
to the nature of post-injection pain sensations, the duration of
the course of local inflammatory reactions. The condition of the
tissues in the injection site was evaluated, the result of palpation
of periodontal tissues, the density of post-injection infiltrate (regenerate)
formed in the area of the osteoplastic material location
were taken into account. To determine the optical density of
the bone (according to the method of Vagin P. V., 2012) and the
nature of the structural changes occurring in it, the methods of
orthopantomography and computed tomography were used. The
criteria for including patients in the study were: diagnosed local
(within 1-3 missing teeth) post-extraction moderate atrophy and/
or deformation of the alveolar part of the jaw: the age of patients
(20-50 years), informed consent of the patient. The exclusion
criteria were severe general somatic diseases: diabetes mellitus,
chronic renal failure, severe anemia, heart and respiratory failure,
oncological diseases, urgent conditions, as well as the patient's refusal
to participate in the study at any stage.
Results and Discussions
One day after injection osteoplasty, the analyzed signs were present
in most of the representatives of the comparison groups
without significant differences. Significant intergroup differences
were detected from the 2nd to the 5th-6th day of treatment and
were registered for all the analyzed signs. Moreover, local postinjection
reactions were more pronounced in the main group,
where combined subcostal administration of osteoplastic drugs
was used. This tissue reaction was predictable for us, because the
proposed method, in addition to using two dissimilar materials,
also included additional traumatic elements: microtunneling and
tissue hypertension with hypercorrecting introduction of osteoplasts.
In addition, local inflammatory reactions were purely local
in nature and did not lead to the development of complications.
At the same time, the treatment method used in the main group
of patients was aimed at implementing the main task of the study
- the formation of a bone regenerate capable of eliminating a
limited defect of the alveolar process. The results obtained on
the 14th day of observation indicated a complete subsiding of local
inflammatory reactions. Against this background, the signs of
bone regenerate formation, more pronounced in the main group,
were visually and palpatory determined in the osteoplasty site.
Here, complete elimination of the deformity after the first stage
of treatment was achieved in 44.73% of patients (against 16.67%,
with p<0.05-in the control).
Long-term treatment results were evaluated using clinical and radiological
examinations. The results of X-ray monitoring of the
effectiveness of injection methods for eliminating post-extraction
deformities of the alveolar process were evaluated by indicators
characterizing the formation of bone regenerate in the area of introduction
of osteoplastic materials, the structure and volume of
the newly formed bone, and the degree of its optical density. Our
comparative study showed that with the combined use of osteoplasts
(PRP and Collapan), radiological symptoms of an increase
in the volume of the cortical bone (having a large-loop structure)
appear already by the end of the first month after the completion
of treatment. After 6 months of observation, this bone regenerate
acquired a distinctive fine-loop structure. According to the
results of the evaluation of the indicators characterizing the optical density of bone tissue in the area of the performed osteoplastic
therapy, it was possible to establish that the most dense and
mineralized bone regenerate became after 3 and 6 months in the
representatives of the main group. Moreover, here the indicators
exceeded the normal level, which is due, in our opinion, to the
combined (osteoinductive and osteoconductive) influence of the
drugs used for treatment. In the control group, less pronounced
results were obtained, inferior to the norm indicators, but significantly
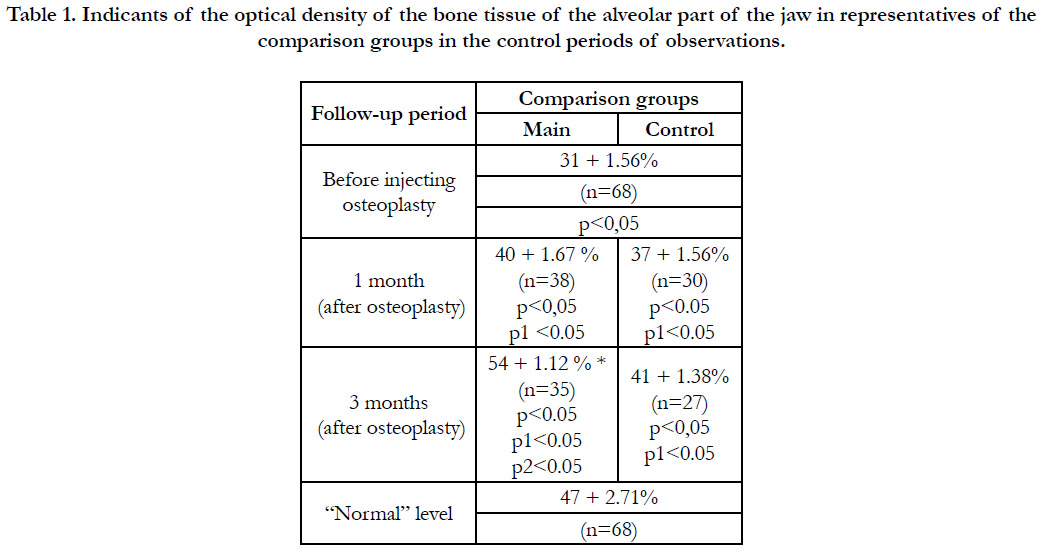
different from the initial values (Table 1).
Table 1. Indicants of the optical density of the bone tissue of
the alveolar part of the jaw in representatives of the comparison
groups in the control periods of observations
Notes:
n - the number of patients in the comparison groups;
p - the reliability of differences in comparison with the "normal"
level;
p1 - the reliability of differences in comparison with the baseline
level;
p2 - the reliability of differences in comparison with the control.
Thus, the results of our experimental and clinical study allowed
us to establish that the injectable use of osteoplastic materials
for local atrophy and deformation of the alveolar part of the jaw
elimination leads to the activation of regenerative reactions and to
the formation of bone regenerate. At the same time, the intensity
of this process increases significantly with the combined use of
drugs that have an osteoinductive and osteoconductive effect of
local action.
Table 1. Indicants of the optical density of the bone tissue of the alveolar part of the jaw in representatives of the comparison groups in the control periods of observations.
Conclusion
The dynamics of the results of clinical examinations of patients
in the comparison groups indicates that local inflammatory reactions
developing in response to injectable subperiosteal injection of osteoplastic materials are moderately pronounced in representatives
of both comparison groups and are completed by 5-7
days of observation. A more striking effect of bone growth is
caused by the combined use of PRP and a synthetic drug (Collapan).
The appearance of a section of newly formed dense tissue
in the injection zone, according to visual-palpatory control,
is determined on the 10th day of the post-injection period and
is traced throughout the entire observation period (6 months).
Combined injectable subperiosteal administration of osteoplastic
materials contributes to a significant increase in the optical density
(mineralization) of bone tissue in the zone of osteoplastic therapy
(by 21%, at p<0.05), during three months, in comparison with the
control (10.0%, at p<0.05), with the formation of a small-cell and
more voluminous (than in the control) bone regenerate.
References
-
[1]. Timofeev AA. Manual on MFS and surgical dentistry. Kiev. 2002.
[2]. Ide S, Ide A. Secrets of the basal implantology. 2011./dr.ihde@implant.com, Munich, Germany.
[3]. Bezrukov SG,Gerasimenko OV, Saenko TS. Results of subcostal injection of osteoplastic materials into the alveolar part of the jaw of experimental animals. Crimean Journal of Experimental and Clinical Medicine. 2018;8(1): 11-15.
[4]. Kalashnikov AV, Zubenko AG, Rudenko IA, Renev KV, Rudenko R I. The first clinical experience of using platelet-rich fibrin gel. Trauma: scientific and practical journal. 2011;129(3):137-140.
[5]. Bashkina AS, ShirokovaLY, Noskov SM. The use of platelet-rich plasma in the relief of pain syndrome of the large trochanter. Traumatology and orthopedics of Russia. 2011;60:57-61.
[6]. Bergeson AG., Tahsjian RZ,Burks RT. Effects ofplatelet-rich fibrin matrix on repair integrity at risk of rotator cuff tears. AmJSports Med. 2011;40(2):286-293.
[7]. Cohen ES. Atlas of cosmetic and reconstructive periodontal surgery, IraqMed. 2011.
[8]. Watson RM, Hobkek JA. Guide to dental implantology, MEDpressinform. 2010.
[9]. Bezrukov SG, Gerasimenko OV, Bezrukov GS, Schepelev AA. Clinical and anthropometric evaluation of the results of treatment of postextraction atrophy of the alveolar process by injection of osteoplastic materials. Crimean therapeutic journal. 2018 (3).