Efficacy of Caudal Epidural Block with 0.2% Ropivacaine in Paediatric Patients Undergoing Laparoscopic Unilateral Hernia Repair: A Prospective Randomized Study
Sweta1*, Yogesh Kumar Manik2, Manish Katiyar3
1 Assistant Professor, Department of Anaesthesia and Critical Care, LLRM Medical College, Meerut, U.P. India.
2 Associate Professor, Department of Anaesthesia and Critical Care, LLRM Medical College, Meerut, U.P. India.
3 Senior Resident, Department of Anaesthesia and Critical Care, LLRM Medical College, Meerut, U.P. India.
*Corresponding Author
Dr. Sweta,
Assistant Professor, Department of Anaesthesia and Critical Care, LLRM Medical College, Meerut, U.P. India.
Tel: 08750933442
E-mail: swetaanae@gmail.com
Received: February 19, 2020; Accepted: March 20, 2020; Published: March 31, 2020
Citation: Sweta, Yogesh Kumar Manik, Manish Katiyar. Efficacy of Caudal Epidural Block with 0.2% Ropivacaine in Paediatric Patients Undergoing Laparoscopic Unilateral Hernia Repair: A Prospective Randomized Study. Int J Anesth Res. 2020;8(2):589-593. doi: dx.doi.org/10.19070/2332-2780-20000117
Copyright: Sweta© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background and Objectives: The assessment and quantification of postoperative pain is more difficult in children than adults. Regional anesthesia and analgesia has shown to provide excellent analgesia and also provide benefits, which extend beyond the perioperative period. Caudal epidural block is a gold standard technique in paediatric lower abdominal surgeries. The aim of this study is to evaluate perioperative effect of caudal epidural block in children undergoing laparoscopic hernia repair surgeries regarding hemodynamic changes in intra-operative period, postoperative pain score, rescue analgesia requirement and any side effects.
Methods: Sixty children aged 2–12 years with ASA grade I or II scheduled for laparoscopic unilateral hernia repair were randomly allocated into two groups: group A (General anaesthesia with caudal block) and group B (General anaesthesia without caudal block). Postoperative pain scores, rescue analgesic requirement, intraoperative hemodynamic changes, any complication related to caudal block were recorded.
Results: All children were comparable regarding demographic profile. There was no statistically significant difference in hemodynamic changes between both the groups. The mean postoperative pain score was significantly lower in group A (2.98 ± 1.08) as compared to group B (3.63 ± 1.49) (p = 0.002). Eleven (36%) subjects in group A and 25 (83%) subjects in group B needed rescue analgesic in postoperative period. The incidence of adverse effects was higher (30%) in group A than group B (13%).
Conclusion: We concluded that caudal bock with 0.2% ropivacaine in paediatric patients provides better analgesia, without significant intraoperative hemodynamic changes.
2.Background
3.Methods
3.1 Statistical analysis
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Paediatric; Ropivacaine; Caudal; Laparoscopic; Regional.
Background
In paediatric patients, though general anaesthesia is the commonly used technique, regional anesthetic technique is often used for intra-operative as well as postoperative pain relief. Caudal epidural block is commonly used as it is a safe, reliable, and easy to administer technique for lower abdominal surgeries [1].
Caudal block allows rapid recovery from anaesthesia, as it decreases the requirement of other systemic anesthetic drugs, with effective postoperative analgesia [2]. This technique is a useful adjunct during general anaesthesia. The quality and level of the caudal block depends upon the dose, volume, and concentration of the injected drug.
In comparison to bupivacaine, ropivacaine is known to have lesser cardiotoxicity and motor blockade, with similar pain relief at equivalent analgesic doses. It is considered to be a better agent for caudal epidural analgesia in children [3-6].
Prophylactic analgesia with local anesthetics is an attractive concept, especially in paediatric practice, because the evaluation of pain can be very challenging in young children [7]. Local anesthetics can be administered safely in contrast to opioids. The global experience with paediatric regional anesthesia is still quite low inspite of good safety records and even the most commonly performed procedure, caudal block represents only 2.5% of all central neuraxial blocks performed [8, 9].
This prospective randomized double blind study was designed to evaluate perioperative effect of caudal epidural block in children undergoing laparoscopic hernia repair regarding intraoperative hemodynamic changes, postoperative pain score, rescue analgesia requirement and any complication related to caudal block.
Methods
After institutional ethical committee approval, sixty children aged 2–12 years of either sex, with ASA grade I or II scheduled for laparoscopic unilateral hernia repair were included in our study.
Patients with history of developmental delay or mental retardation, history of Diabetes mellitus type I, known allergy or contraindication to any local anesthetics, known congenital anomaly in the inguinal region, infection at local site were excluded from the study.
Patients were randomly allocated into two groups using a computer generated coding system.
Group A: (General anaesthesia with caudal block with 0.2% Ropivacaine 1ml/kg).
Group B: (General anaesthesia without caudal block).
All the patients scheduled for surgery visited a day prior to surgery. A thorough pre- anesthetic check up was done including the detailed history, systemic and airway examination. Specific questions were asked related to previous anesthetic exposure of any surgery and any major cardiovascular, neurological or respiratory illness. All the necessary routine investigations were done as per institutional protocol. Parents of children were informed and explained about the procedure and any doubts or apprehensions were clarified. A written informed consent was obtained from the parents. No premedication was advised.
On the day of surgery, children were monitored by means of ECG, pulse oximeter, and noninvasive blood pressure after shifting to the operating room table. In all patients intra-venous (i.v.) cannula was secured in nondominating forearm. After preoxygenation for 3 min, induction was done with 50% oxygen 50% nitrous oxide and sevoflurane using Jackson Rees circuit. Induction was carried out by increasing the concentration of sevoflurane in stepwise manner starting from 1% and gradually increasing to 5-6% i.e. 1% every 6-8 breaths. After induction Injection 1 μg/ kg fentanyl was administered intravenously and adequate size endotracheal tube was placed and secured in position. In group A, children received caudal block with 0.2% ropivacaine at 1 ml/kg. For caudal block, the sacral hiatus was identified and a 22 G short length caudal needle ( Epican short length caudal needle, B.Braun) was passed through the sacrococcygeal ligament to inject a local anesthetic after confirmation of space by loss of resistance technique. After caudal block the patient was turned into supine position, surgeon was allowed to clean and drape. General anaesthesia was maintained with oxygen 40%, nitrous oxide 60% and isoflurane (0.6% -1%). Intra-operatively injection atracurium was used as skeletal muscle relaxant. No other narcotic, analgesic, sedative, or antiemetic was used intraoperatively.
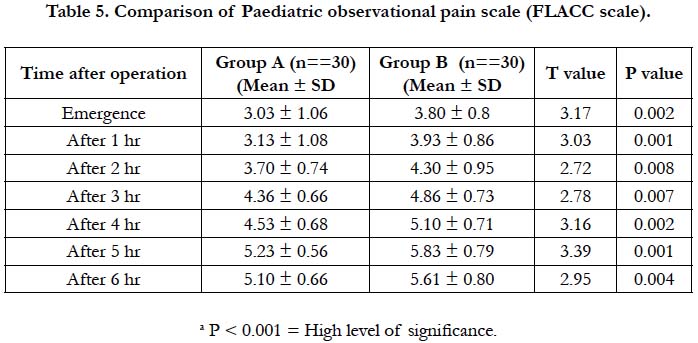
During anaesthesia patients were monitored by ECG, pulse oximetry, capnography and non-invasive measurements of arterial pressure. Parameters were recorded 1 min after creation of carboperitoneum and then every 10 min until the surgery was over. After surgery patients were shifted to surgery intensive care unit for further observation and monitoring. Post -operative pain by pediatric observational pain scale score (FLACC score) was determined on emergence from anaesthesia and 1,2,3,4,5,6 hour until the first dose of rescue analgesia was given in form of paracetamol 15mg/kg when score was ≥4. Other adverse effects such as nausea, vomiting, respiratory depression, bradycardia, hypotension, urinary retention, facial flushing and pruritus were also observed. The observer and parents of the children were blinded to the technique.
Postoperative pain was assessed using the Faces Legs Activity Cry Consolability tool (FLACC, 0- 10) as in the table given below:
Sample size was calculated based on pilot study on 10 patients in both the groups. With 95% confidence interval and 80% power of study, sample size was determined to be 60 with 30 patients in each group.
Data was statistically analyzed using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical Analysis Software. Quantitative data were described as mean ± SD and qualitative data as frequency and proportions. The chi square-test was used to compare qualitative data between two groups while Student t-test was used for quantitative data. P values of 0.05 or less were considered significant.
Results
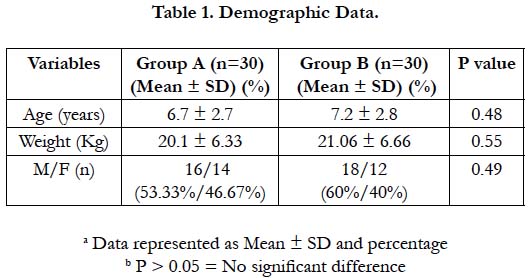
All children were comparable in terms of demographic profile (p>0.05). The mean age of the patients in group A (6.7 ± 2.7) was comparable to group B (7.2 ± 2.8 yrs). The mean weight of the patients in group A and group B was 20.1 + 6.33 and 21.06 +6.6 kg respectively. There were 14 females and 16 Males in group A as compared to 12 females and 18 males in group B. [Table 1]
Both group A and B were comparable in respect to baseline heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, oxygen saturation and end tidal carbon dioxide (p>0.05).
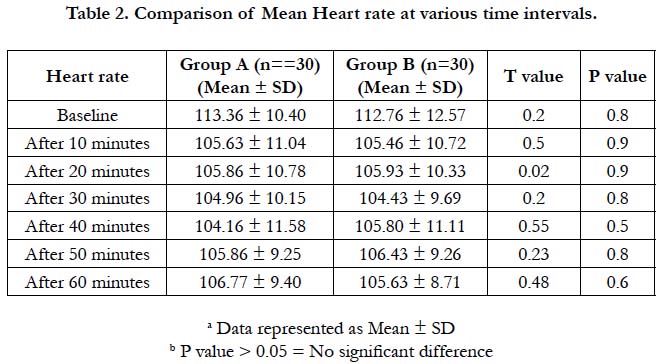
The mean heart rate values were comparable in both the groups at entire time interval (p> 0.05). None of the patients in either group required treatment with atropine as the heart rate never fell below 60 beats per minute [Table 2].
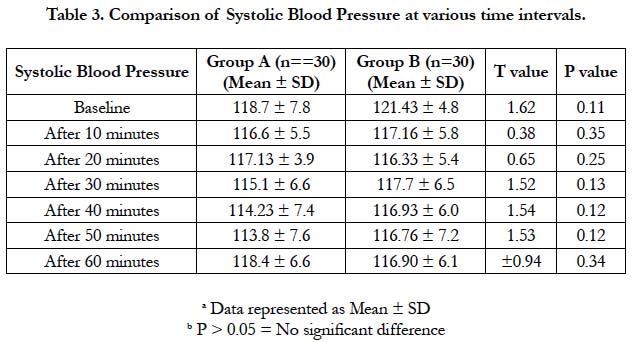
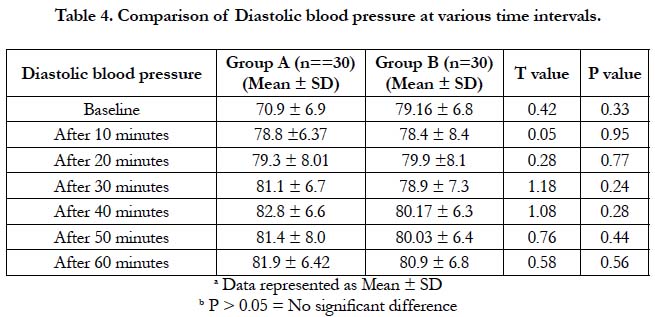
There was no statistically significant difference in mean systolic and diastolic pressures at entire time interval. (p>0.05) [Table 3 and 4].
The postoperative pain score was significantly lower in group A (2.98 ± 1.08) in comparison to group B (3.63 ± 1.49) (p = 0.002). 11 (36%) patients in group A and 25 (83%) patients in group B needed rescue analgesics postoperatively [Table 5].
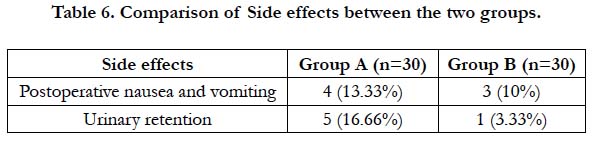
The incidence of adverse effects was higher in group A (30%) than group B (13%). 5 patients in group A developed urinary retention and 4 patients experienced nausea or vomiting. In group B urinary retention was present in 1 patient and nausea or vomiting was present in 3 patients. [Table 6]
Discussion
Management of postoperative pain is a great challenge to the clinicians, especially in paediatric age group. If not treated it may result into various physiological changes, including rise in heart rate, blood pressure, restricted physical activity and sleepless nights. Attenuation of perioperative Pathophysiology that occurs during the surgery through reduction of nociceptive input into the CNS and optimization of postoperative analgesia may decrease complication and facilitates recovery of the patients in the immediate postoperative period and after discharge from the hospital.
Many options are available for treatment of postoperative pain, including systemic (opioids and non opioids) analgesics and regional (neuraxial and peripheral) analgesic techniques. Neuraxial blockade especially caudal epidural blocks assume an integral role in the management of lower abdominal surgeries in paediatric patients as they are used not only to provide surgical analgesia but can be used in the postoperative period to provide effective pain relief.
We decided to use Ropivacaine in our study because in comparison to bupivacaine, it has a wider margin of safety, less motor blockade, less cardiovascular or neurological toxicity. It can be safely used for regional anesthesia and analgesia in ambulatory setting of pediatric patients [3, 8]. Ivani et al., reported a significantly increased duration of analgesia for ropivacaine in comparison to bupivacaine. While comparing ropivacaine with bupivacaine for pediatric caudal block in 245 children they found that the mean time to first analgesia after bupivacaine was earlier than that after ropivacaine [10].
Kay et al., [11] was one of the early advocates of caudal bupivacaine to provide intra- and postoperative analgesia for circumcision in day cases, and Lunn et al., [12] demonstrated the superiority of caudal block over intramuscular morphine for postoperative analgesia.
Cheon et al., [13] who compared caudal block with local infiltration in children undergoing inguinal herniorrhaphy noticed that children in the caudal group did not need rescue analgesic; however, in that study postoperative pain was assessed for 2 h only. In our study, 11 patients in group required rescue analgesia postoperative period.
Also, a meta-analysis comparing caudal block with noncaudal regional techniques for inguinal surgeries in children found that caudal block might be a better analgesic in early and late postoperative periods, but with a significant risk for motor block and urinary retention which was similar to our study, in which postoperative pain score was significantly lower in group A (2.98±1.08) in comparison to group B (3.63±1.49) (p= 0.002) although urinary retention was higher in caudal group [14].
However, Bramwell et al., [15] noted a significantly greater consumption of analgesic drugs between 2 and 8 hours postoperatively in patients who received caudal analgesia in comparison to those given intramuscular dihydrocodeine while in our study, there was lesser consumption of analgesic drug within 6 hours of postoperative period.
Yeoman et al., [16] demonstrated a 42% incidence of urinary retention at 6 hours in patients who received caudal block, which was greater than our study in which only 36% patients developed urinary retention. Moores et al., [17] reported 11% incidence of unsteadiness of gait in the caudal group at 4 hours while no patient in our study developed such type of complication.
Conclusion
We concluded from our study that caudal block with 0.2 % ropivacaine provided effective postoperative analgesia following laparoscopic surgery in paediatric patients. It also provided better intraoperative hemodynamic stability and less postoperative analgesic requirement.
References
- De Beer DA, Thomas ML. Caudal additives in children—solutions or problems?. BJA. 2003 Apr 1;90(4):487-98.
- Sethna NF, Berde CB. Pediatric Regional Anaesthesia. 4th ed. Gregory GA, editor. Pediatric Anaesthesia. New York: Churchill Livingstone Inc; 2003. p. 267–8.
- Reiz S, Häggmark S, Johansson G, Nath S. Cardiotoxicity of ropivacaine: A new amide local anaesthetic agent. Acta Anaesthesiol Scand. 1989 Feb;33(2):93-8.Pubmed PMID: 2922986.
- Knudsen K, Beckman Suukula M, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997 May;78(5):507-14. Pubmed PMID: 9175963.
- Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. AnesthAnalg. 1989 Nov;69(5):563-9. Pubmed PMID: 2679230.
- McClure JH. Ropivacaine. Br J Anaesth. 1996 Feb 1;76(2):300-7.
- Jöhr M. Regional anaesthesia in neonates, infants and children: an educational review. Eur J Anaesthesiol. 015 May;32(5):289-97.Pubmed PMID: 25693139.
- Cook TM, Counsell D, Wildsmith JA. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth. 2009 Feb;102(2):179-90.Pubmed PMID: 19139027.
- Crellin D, Sullivan TP, Babl FE, O'Sullivan R, Hutchinson A. Analysis of the validation of existing behavioral pain and distress scales for use in the procedural setting. Paediatr Anaesth. 2007 Aug;17(8):720-33. Pubmed PMID: 17596217.
- Ivani G, Lampugnani E, Torre M, Calevo Maria G, DeNegri P, Borrometi F, et al. Comparison of ropivacaine with bupivacaine for paediatric caudal block. Br J Anaesth. 1998 Aug;81(2):247-8. Pubmed PMID: 9813532.
- Kay B. Caudal block for post‐operative pain relief in children. Anaesthesia. 1974 Sep;29(5):610-1.
- Lunn JN. Postoperative analgesia after circumcision. A randomized comparison between caudal analgesia and intramuscular morphine in boys. Anaesthesia. 1979 Jun;34(6):552-4. Pubmed PMID: 484815.
- Cheon JK, Park CH, Hwang KT, Choi BY. A comparison between caudal block versus splash block for postoperative analgesia following inguinal herniorrhaphy in children. Korean J Anesthesiol. 2011 Apr;60(4):255-9. Pubmed PMID: 21602975.
- Shanthanna H, Singh B, Guyatt G. A systematic review and meta-analysis of caudal block as compared to noncaudal regional techniques for inguinal surgeries in children. Biomed Res Int. 2014;2014:890626. Pubmed PMID: 25162033.
- Bramwell RG, Bullen C, Radford P. Caudal block for postoperative analgesia in children. Anaesthesia. 1982 Oct;37(10):1024-8.
- Yeoman PM, Cooke R, Hain WR. Penile block for circumscision? A comparison with caudal blockade. Anaesthesia. 1983 Sep;38(9):862-6. Pubmed PMID: 6625133.
- Moores MA, JG Wandless JG, D Fell. Paediatric postoperative analgesia. A comparison of rectal diclofenac with caudal bupivacaine after inguinal herniotomy. Anaesthesia. 1990 Feb;45(2):156-8.Pubmed PMID: 2321721.